Access to Health Care for Childhood Disability
Whilst Australia promotes our healthcare system as one of the ‘best in the world1‘, it’s seriously broken and monopolised by the Australian Medical Association (AMA). With only 2 registered Paediatricians’ in Australia, access to a paediatrician, is a massive barrier to obtain a formal diagnosis in this country. Figure 1, provides an overview of the number of practicing specialists in Australia who may be involved in treating children with Autism and ADHD. With the exception of Paediatricians who are solely dedicated to treating children, these health professionals can treat anyone at any stage, health or development condition.
Like many areas in Australia, the medical profession is currently experiencing a major skill shortage and given that a qualified Paediatrician is required to formally diagnose childhood development disorders such as ADHD, Autism, Dyslexia and Dysgraphia, the sheer lack of qualified Paediatrician’s trained in Australia is a major barrier to accessing treatment, intervention and a diagnosis.

So why do i say that the Australian Medical Association (AMA) is actively campaigning against addressing this critical skill gap? Because recently the GO8 released a national round table policy working group to address the critical gaps in Medical specialists in Australia. They made a recommendation to the Federal Government, to increase the number of Government Supported university placements by 1,000 each year to address this skill gap. The AMA, actively campaigned against the increase in doctor training positions in Australia, citing ‘that the funding would be better placed elsewhere3‘. We as Australian’s need to think about the role of the AMA, whilst they promote themselves as the ‘Peak Professional Body’ for Doctors in Australia4, which is a fancy way of saying that the AMA is first and foremost the ‘union’ for Doctors in Australia and like all other union bodies, one of their primary objectives is to ensure that Doctors and Specialist places in Australia are regulated to keep the number of practitioners low and the demand and prices they can charge high.
So why is the medical shortage an issue for kids?
Why is the medical issue compounded for children? Whilst a speech, occupational therapist and psychologist can formally diagnose both ADHD and Autism, if your child requires medication to support their treatment, the only specialist who can formally diagnose and prescribe ADHD medication is a paediatrician. Concurrently, the interventions that are required for a child with a neurodiverse condition are predominantly allied health, these services are extremely costly, however a GP or Paediatrician can develop a Mental Health Plan which will provide greater rebates to offset some of the costs of treatment and require repeat visits to a GP to create and update the plan.
Also, concurrently to help us navigate my daughters challenges, we relied on our GP and a referral to a paediatrician, a process that took 3 years to get into a paediatrician initially due to the demand on this specialty.
So how much does treatment cost for Autism and ADHD?
The costs for providing treatment for childhood diagnostic conditions is expensive, take my daughter for example, she received a dual Autism and ADHD diagnosis, in order to provide her with the necessary supports she requires, we are out of pocket significant sums of money every year. The below figure, provides an overview of the recommended treatment plan and out of pocket costs for this.
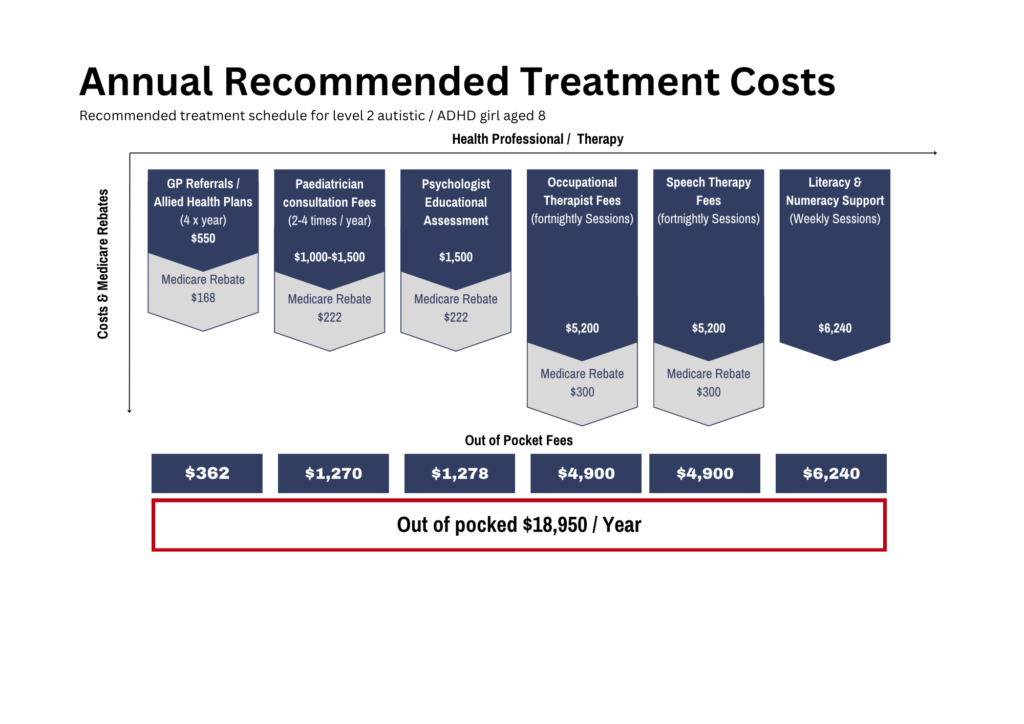
Pragmatically, there is no way my daughter can undertake therapies at the frequency we were recommended due to the cognitive load, logistics and impact on her participation in school, but if we were to follow all treatments, we would be out of pocket $18,000 every year. Whilst in hindsight i could have sought an alternative diagnostic pathway for my child and not relied solely on a Paediatrician, the alternative pathways aren’t as enticing either, from speaking with friends and colleagues, this could have resulted in years of unnecessary therapy from allied health (e..g Speech therapists, occupational therapists, psychologists), however the limitation in this is that these professionals only specialise in individual modalities and you can find yourself wasting countless $$ and loads of time focusing on one therapy and not addressing the root cause of the issue.
So are there cheaper alternatives to treatment and diagnosis?
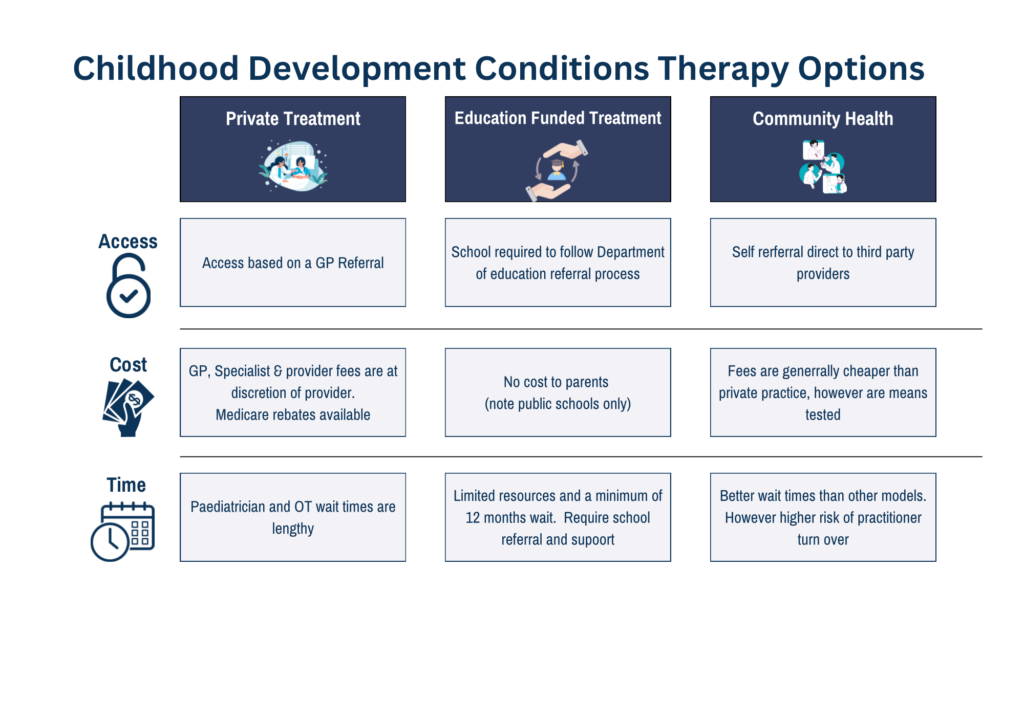
Whilst I would love to say ‘Yes’, the reality is that there aren’t cheaper approaches to obtaining treatment for Childhood development conditions. Practically speaking, there are potentially 3 models of care Available in Australia, of which all have significant limitations. The below figure provides a summary of the models and the access, costs and time limitations of each system. Whilst in theory, Community Health offers the best proposition, this is means tested and a family income above $118,000 is deemed as ‘high income’ and attracts full fees for service.