Since 2021 the Victorian Government has been promoting their ‘investment of $1.6 billion to support children with a disability in State Government Schools. The Department has advised that this program will be delivered via a tiered funding modelin the State Education System. Underpinning this investment is the ‘Disability Inclusion Policy’ that claims that schools can access 3 levels of funding to support children with additional needs at school.
Whilst the Disability Inclusion Policy is supposed to be designed to support children who are protected under the Equal Opportunity Act and the Disability Standards for Education, access to this policy is extremely complex and could be argued is discriminatory.
Access to the Disability Inclusion Profile
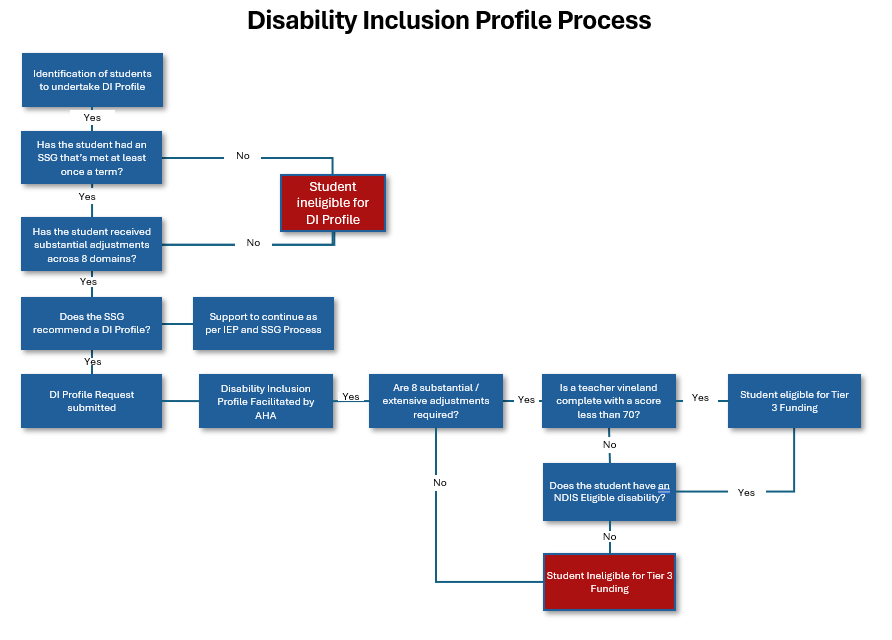
To access student level disability supports, the Departments policy prescribes that schools can apply for a Disability Inclusion Profile. To access this process, which is delivered via a Government Contractor, students are required to have:
- A Student Support Group that meets once a term.
- Be included in the Nationally Consistent Collection of Data for Students with a Disability
- Evidence of Supplementary, substantial or Extensive Adjustments for a period of 10 weeks.
Whilst in principle, this Policy and investment is sound, when you understand and analyse the pre-requisites for students to access this profile and support, it is apparent that the system is floored and could be argued, discriminatory.
Issues with Access to Student Level Profile
Based on analysis of the Department of Education’s Disability Inclusion Policy, resources and guidance which has included reviewing Training provided on the ARC Website, there appears to be some fundamental issues with this policy. Especially, when you overlay this policy and the Equal Opportunity Act (Victoria) and the Disability Standards in Education (Commonwealth) legislation. The below table provides a summary of these issues as they stand today.
| Pre-Requisite | Issues with the pre-requisite | Discussion / Discriminatory Elements |
|---|---|---|
| Student Support Group | 1. It is not mandatory for students with a disability to have a Student Support Group 2. The SSG Policy Does not mandate an SSG unless a student is in out of home care or on the program for students with a disability. An SSG is only ‘strongly encouraged’ per the policy and as such, access to an SSG is only available should the school proactively seek to establish an SSG or parents request an SSG. | As there is no mandate for an SSG for all students with a disability and require accommodations to enable them to take part in education, this is indirectly discriminating. The Disability Standards in Education (Cth) and Equal Opportunity Act (Vic) provides a concise definition of a disability. Both statutes also prescribe that those who are protected under the legislation, are entitled to reasonable adjustments. |
| Access to SSG | An SSG Is not mandatory for students protected under legislative disability protections. A decision to pursuing a Disability Profile is to made by the SSG. To date, there has been no formal correspondence issued to parents to notify of this policy. The failure to inform parents and carers that this policy is available will result in a failure to explore a child’s eligibility. | As the Disability Profile is not mandatory for all students, and the decision to pursue is to be determined by the Student Support Group, it is solely at the discretion of the school leadership team to inform parents and carers this policy is available. There has been no Departmental communication issued to parents and carers that this process is available to support children with additional needs. |
| Student included in NCCD | Students are required to receive adjustments as per the Nationally Consistent Collection of Data. | There is no correlation between the Nationally Consistency Collection of Data requirements and the requirements for schools to establish an SSG. Parents and carers have no visibility of what ‘adjustments’ the school is reporting to the NCCD for their child. The Individual Education Plan and SSG Policies make no mention of what medical evidence is required to determine a students ‘required level of adjustment and often it is at the discretion of the SSG to determine what adjustments are required. In the absence of a standard ‘education capabilities’ process to seek medical advice on ‘reasonable adjustments’, adjustments are at the discretion and capability of the school. Whilst the DI Policy references the NCCCD Adjustment levels, due to multiple variables, it is highly probable that schools are providing a far lower level of adjustment that is medically required for children with a disability. |
| Supporting Evidence for Disability Inclusion | The policy makes clear that no new medical evidence is required. The policy references the School Wide Adjustments Guidance document which outlines what supporting information can assist. The School Wide Adjustments guidance references a ‘General Medical Advice’ form which is available under the ‘Health Care Needs Policy. | There is no link between the ‘Health Care Needs Policy, the SSG Policy, the IEP Policy or the Duty of Care policy. None of the listed policies make mentioned to a standardised process to obtain current medical information for any student with a disability. Failure to request recommendations from a student’s health care providers regarding the adjustments a student requires is failing to make reasonable enquiry to support a child. The evidence required for a disability profile is not providing adequate consideration to an individual student’s needs and is instead relying on Teachers and the Australian Health Professionals (contractor facilitating DI profiles). The failure to receive student specific advice regarding the adjustments required by a student with a disability is clear evidence of a school failing to discharge their duty of care. |
| Mandatory Requirements for Student Specific Funding (Tier 3) | For schools and students to access additional funding for ‘Reasonable Adjustments’, in addition to having a Disability Inclusion Profile undertaken they must meet the following 3 criteria: 1. Evidence of 8 Substantial or Extensive Adjustments reported in the NCCD for a period of 8 weeks or more. 2. A Vineland Teacher Score of less than 70 3. If a Vineland score of is greater than 70, they must have a disability covered via the NDIS. | The eligibility requirements in themselves are discriminatory based on the following: Substantial / Extensive Adjustments – The process to identify what adjustments are required is not based on medical evidence, instead it is at the discretion of the school and SSG. Due to schools budgets, it is inevitable that the least costly and simplest adjustments will be implemented. Vineland Teacher Score – This assessment measures only the behavioral and social domains, yet there are 32 domains recognised by DET for the Disability Inclusion Profile. This assessment and process are designed to accommodate and prioritize intervention for Children with behaviour issues over learning issues. Concurrently, the literature pertaining to girls and neurodiversity highlights masking or camouflaging their neurodiverse symptoms is heightened in girls. By design, this tool as the sole measure for access to funding, is discriminatory towards girls. NDIS Disability – There are countless disorders that impact a child’s ability to learn that are not eligible for NDIS. For example, a child with Dyslexia and dysgraphia would not qualify for NDIS, yet their ‘disability’ is protected by law, and the education system is failing to allow for these children to receive adequate support. |
Delivery of the Disability Inclusion Profile Costs
As part of the transition from the former policy ‘Program for Students with a Disability’ to the Current program ‘Disability Inclusion Policy’ it appears that the Department has engaged Australian Healthcare Associates (AHA) to develop a Functional Needs Assessment Pilot at a cost of $879,000. From information obtained on AHA’s website, this program developed a Functional Needs Assessment Tool (FNA Tool) on behalf of the Department and according to AHA’s website, 109 FNA’s were developed in Victoria during this time.
Whilst the Formal ‘Disability Inclusion Policy’ commenced in Victoria under a phased implementation plan, with a Closed Tender contract awarded to AHA to the value of $33,868,000 to provide Disability Inclusion Facilitators. In June 2023 The Victorian Attorney General’s Office (VAGO) undertook an Audit of the Disability Inclusion Profile Implementation. Some key findings from this report include:
- Tier 2 funding is to be calculated by the school’s Student Resource Package. This funding is provided to schools based on Family Characteristics to allocate funding levels to schools. It has been unable to ascertained how the ‘actual number’ of students with a disability at individual school will impact the tier 2 funding allocated.
- The Department has employed 8-10 people in the ‘School Supports Division in the roles of ‘DI Implementation Manager and DI Senior Implementation Managers and 25 Education Improvement Leaders – Diverse Learners in the ‘School Improvement Division’ 35 roles dedicated to the implementation of the Disability Inclusion Profile
- At a local level, the Department has employed 1 Regional Inclusion Outreach Coaching Coordinator and 4-13 Inclusion Outreach Coaches, per region. Based on 4 region’s within the Department this would equate to 5-56 employees at a regional level
- In addition to the above, the Department has spent $39,386,000 with the Australian Healthcare Associates to engage Disability Inclusion Facilitators
Despite employing between 40-91 employees within the Department to administer the Policy plus the contracted costs for the Disability Inclusion Facilitators, as at December 2022, the Department had only completed 881 Disability Inclusion Profiles.
| Contract Ref | Contract Dates | Contract Title | Provider | Estimated contract amount |
|---|---|---|---|---|
| CR33098 | Jan 2014 – Dec 2017 | Provide Administration for Program for Students with a Disability | Australian Healthcare Associates | $6,616,395 |
| CW3707 | Jan 2015 – Dec 2018 | Program for Students with a Disability Assessment | Assessments Australia | $22,160,797 |
| CW21810 | Jan 2018 – Dec 2019 | Program for students with a disability | Australian Healthcare Associates | $3,964,442 |
| CW27740 | May 2018 – Feb 2019 | Functional Needs Assessment Pilot | Australian Healthcare Associates | $879,000 |
| CW385582 | July 21 – Dec 24 | Disability Inclusion Program Facilitators | Australian Healthcare Associates | $33,868,000 |
| CW45394 | Jan 22 – Dec 24 | Program for students with a disability administration | Australian Healthcare Associates | $5,518,000 |
| $72,521,634 |
How are reasonable adjustments determined?
Good question, from everything i have seen to date, the FNA Tool is used to assess a students strengths, however all information available on how this relies on the opinions and experiences of teachers with a component for parents to complete and contribute. The ‘Disability Inclusion Faciltiators’ will then attend countless meetings with the school and parents to facilitate a students strengths and weaknesses. It doesn’t appear that the FNA Tool is published to the community, but what is published, is that the DI Process does not require additional medical information.
At no stage in this entire process to determine what adjustments a child requires, are targeted questions asked by the Department, regarding what best adjustments are required to support a child, from their own treating medical team.
As a parent of a child with Autism, I have no idea what my child needs at school, I have no medical training or experience and concurrently, teachers are not qualified to determine what best adjustments are required either, they are experts in teaching, but have no medical training.
Why are we not asking for medical evidence as the first point of call to assess the medical opinion of what adjustments a child needs to support them in the learning environment?
Could this be done better? YES
Coming from the corporate sector where the Human Resources and Safety Departments oversee policies including Reasonable Adjustments and Return to Work Programs under the Workers Compensation Act’s, these policies are administered in a far simpler and far more ‘evidenced based approach. The first step in either of these processes is to write to the Workers Treating Medical Practitioner, with the workers permission to find out what adjustments a worker requires. Only once this information is provided, will an employer review the medical information at hand, review the inherent requirements of the role, and then determine what adjustments are reasonable to accomodate.
In fact, when it comes to the Department of Education’s own ‘Employee Reasonable Adjustment Policy’, they specifically reference to seek medical advice from a suitably qualified professional using the Job Access process in the Departments Disability and Reasonable Adjustments Policy. So why, does the Department seek to follow a sound legal and evidence based process for their own employees, yet when it comes to students, create a process that actively avoids seeking medical advice, yet has employed in excess of 56 ‘corporate jobs’ and spend over $39 million with consultants to administer this process?
Wouldn’t these resources and funds be better spent seeking expert medical advice, improving access to student support services at schools for the diagnosis of children as required and make decisions on adjustments based on medical evidence which is in the best interest of the community?